Inside Telehealth
The SteadyMD Blog
March 17, 2025
How SteadyMD is Leading the Way in Responsible Antibiotic Prescribing
As SteadyMD continues to grow, we’ve not only expanded our scope of care but also leveraged data to track outcomes across millions of patients—all while maintaining our focus on high-quality...May 6, 2024
SteadyMD and Bridge Partner to Make Health Insurance Acceptance for Telehealth Consultations Effortless
New partnership will empower digital health companies to quickly and easily accept health insurance, lowering patient out-of-pocket costsFebruary 20, 2024
Telemedicine Effective for Chronic Conditions, New SteadyMD Survey Finds
Annual clinician survey addresses a range of topics related to the adoption, perception, and practice of telehealth.January 5, 2024
Join us at the 2024 ViVE Conference
SteadyMD will be participating in the 2024 ViVE Conference in Los Angeles. Let’s schedule some time to meet.December 21, 2023
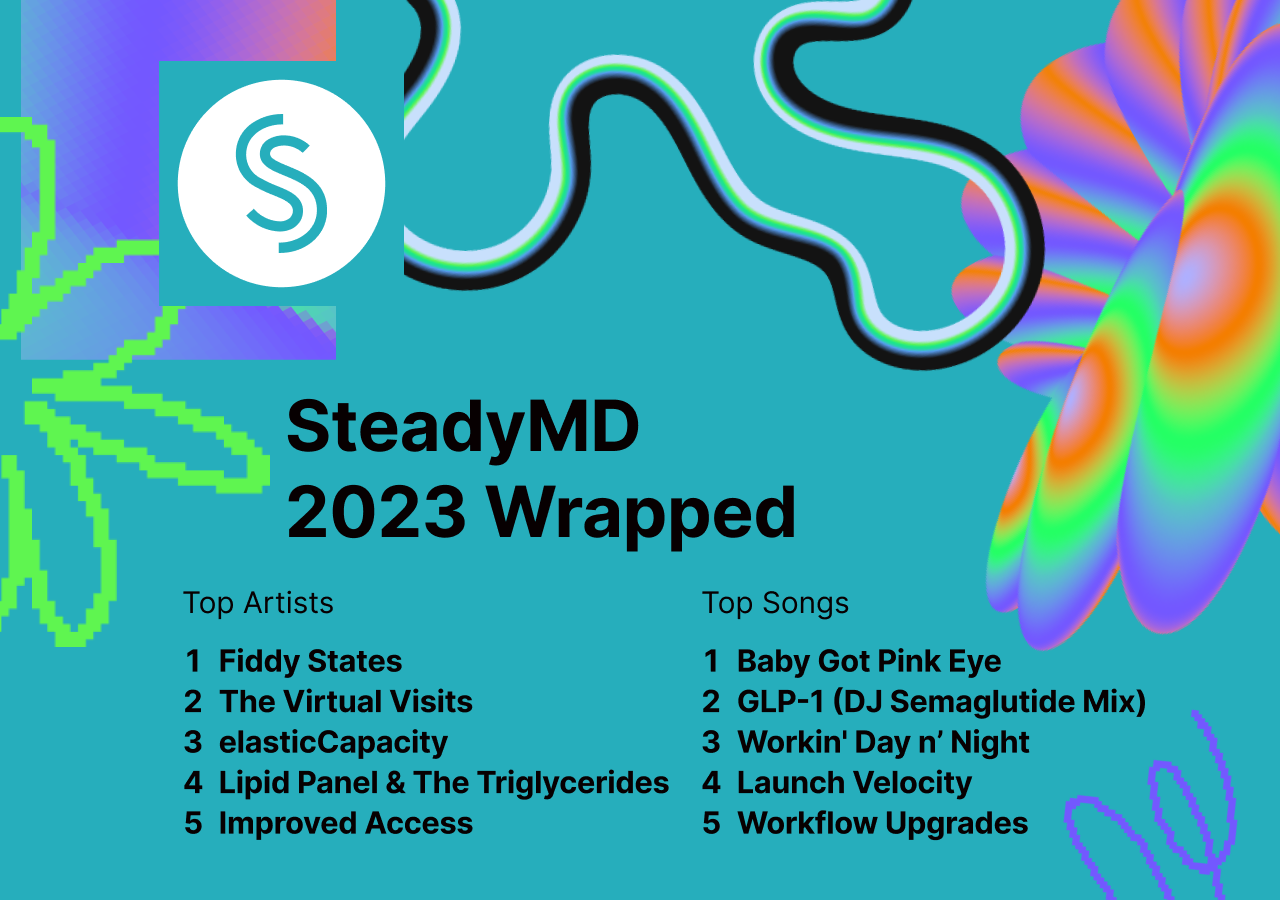
SteadyMD’s 2023 Wrapped
We’ve achieved a lot this year in the service of patients, our customers and our clinicians. Here are the highlights.December 7, 2023
SteadyMD Report Identifies 3 Trends That Will Shape Healthcare Landscape in 2024
Clinician shortages, telehealth demand and GLP-1 treatment will require innovative technology solutions.October 9, 2023
98point6 Technologies Collaborates with SteadyMD to Offer Comprehensive Virtual Care Solution to Healthcare Organizations
98point6 Technologies, a leader in virtual care software, today announced a new strategic partnership with B2B telehealth infrastructure provider, SteadyMD.September 6, 2023
Koa Health and SteadyMD partner to power a comprehensive approach to mental health care across the continuum
This new partnership will make mental healthcare more accessible for organizations supporting workforce wellbeing.August 29, 2023
SteadyMD Supports Amazon Clinic’s Expansion of Telehealth to All 50 States
SteadyMD is delighted to announce that its trusted telehealth services are now available to Amazon Clinic customers in all 50 states! As one of its first partners, we’re honored to expand access to quality virtual care to Amazon Clinic patients nationwide.March 27, 2023